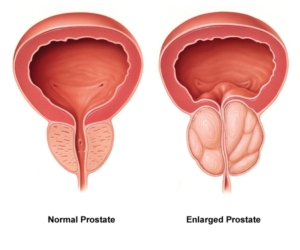
Benign prostatic hyperplasia
Benign prostatic hyperplasia (BPH) is a slow progressing enlargement of the male prostatic gland. It is one of the the top 10 most diagnosed conditions in men over the age of 50 years1. More than half of men in their 60s and up to 90% of men in their 70s and 80s suffer from Lower Urinary Tract Symptoms (LUTS) caused by BPH.2
Why the prostate grows with age is still not fully understood. The enlargement is explained by a multi-factorial constellation of characteristics and risk factors such as: genetic factors, hormonal changes, secondary inflammation and scarring within the gland, diet, overweight and its relation to the metabolic syndrome, and anatomical changes.
All these events can be observed during the aging process.
Many urologists and researchers interpret the inflammatory process as a possible underlying mechanism for both the development of BPH and symptoms related to CP/CPPS and prostate cancer as well.
Lower Urinary Tract Symptoms related to BPH
- Need to urinate more often, both day and night (urgency)
- Weak urine stream or a stream that stops and starts
- Inability to completely empty the bladder
- Dribbling at the end of urination
A Swedish study on 3345 men suffering from Lower Urinary Tract Symptoms (LUTS) showed that 37% of these men mentioned that these symptoms negatively affected their quality of life- 77% answered that their relationship was negatively affected.3
Sources:
1. Fenter et al Am J Manag Care 2006.
2. National Institute of Diabetes and Digestive and Kidney Diseases 2006.
3. Stranne J et al. Scandinavian Journal of Urology and Nephrology 2009;43:199-205.
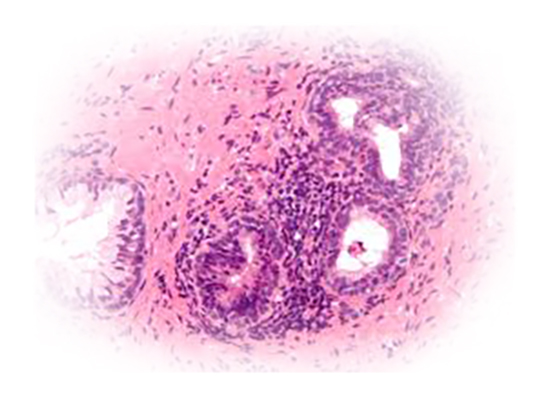
Chronic nonbacterial prostatitis
Chronic nonbacterial prostatitis or chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is a pelvic pain condition in men occurring from around 20 years of age. Inflammation can be detected in patients, but is not required for the diagnosis. Symptoms like pelvic pain, painful voiding and ejaculation, disturbed sexual functions are common, often resulting in a significant impact on quality of life. Professor J Curtis Nickel, Kingston, Ontario, Canada, reported at the EAU annual meeting 2008 in Milan that the annual cost of a prostatitis patient exceeds that of a patient with type 1 diabetes. He also stated that the quality of life of a man with prostatitis is similar to patients with heart failures or acute Crohn’s disease.
Japan, Korea, Germany, Hungary and China are currently the only countries worldwide, where a pharmaceutical product is approved by the national health authorities to treat the diseases; Chronic Prostatitis and Chronic Pelvic Pain Syndrome. Cernitin™ pollen extract (API) is used to treat these conditions.
In all other countries there is no medical treatment approved for the doctor to prescribe, when trying to relieve patients from the often very painful conditions of CP and CPPS. NSAID, alpha-blockers and antibiotics are frequently prescribed instead, with questionable results. Thus, there is an obvious medical need for more effective medicine that can alleviate symptoms of CP and CPPS.
With a reported prevalence from 2.2% to 9.7% and a mean prevalence of 8.2%1 CP/CPPS still constitutes a considerable white spot on the urology map and causes a lot of suffering for patients and frustration among doctors not having efficient solutions to alleviate the patient’s symptoms.
Sources:
1. G. Magistro et al. European Urology 69 (2016) 286-297.
2. F. Wagenlehner et al. European Urology 56 (2009) 544-551.
